
| VEIN DESEASE | |||
| Our vein specialists focus on providing you with the expert care you need and deserve. We don’t just alleviate your symptoms in the short-term. At Texas Vascular and Vein Centers, we’re dedicated to treating the underlying cause of your vein disease, not just the symptoms. Our vein doctors work closely with you to fully understand your problems and accurately identify the true cause of your vein disease. We take the time to help you understand the best vein treatments and lifestyle changes you can make so you can get back to looking and feeling healthy in the long-run | |||
| Varicose Vein | The most common venous conditions are spider and varicose veins, however both can lead to much more serious conditions, including blood clots that form in the superficial and deep veins (aka Superficial and Deep Vein Thrombosis). Spider and Varicose veins can also be a sign of Chronic Venous Insufficiency. If you would like to learn even more about various types of vein disease, check out the book Healthy Veins…Healthy Legs or talk to a vein care specialist. Vein disorders are not always visible; diagnostic techniques are important tools in determining the cause and severity of the problem. If you’re worried about a possible venous disorder, you should seek professional medical advice from a vein care specialist. |
Spider Vein | Spider veins (also called telangiectasias) are small superficial blood vessels in the skin. They get their name because their appearance is similar to that of a spider web. They most commonly appear as blue or purple spider web-like patterns on the inner and outer thighs, calves, back of the knees and the ankle area. Underlying vein disease can be the tip of the iceberg. Some people complain of warmth or discomfort over spider patterns. Do your spider veins or profession indicate high risk factors for vein disease? |
| Bulging Vein | If you notice bulging veins, you have a significant medical condition. Bulging indicates vein dilation. Constant dilation causes vein walls to weaken, leading to further damage. This includes swelling with tissue damage, permanent pigment changes and even ulceration and/or lymphedema. Untreated, vein swelling causes fluid with red cells to continue seeping through weakened vein walls. This pooling results in swelling of the lower leg. Tissue damage results over time and may lead to skin break down, creating an ulcer. Schedule an appointment with our friendly team if bulging veins are becoming too obvious to ignore or if you are suffering from aching or fullness as the day progresses. Treating Bad Veins Before they Get Worse Bulging veins are a sign of venous insufficiency. Allowing signs like bulging veins and ankle swelling to go untreated can lead to further changes that affect your quality of life. Stop wondering about bulging veins. Visit our Knowledge Center to see patient resources that help you identify and treat your vein issues. |
Skin Changes | Your Dry Skin Changes May be a Sign of Vein Disease If you’re experiencing skin changes like dry skin on your lower legs, extremely itchy dry skin, or dry flaky skin on lower legs, it could be a sign of the vein disease, Chronic Venous Insufficiency (CVI). Vein disease causes your veins to dilate and become unsightly and painfully varicose. If you have vein disease, no amount of lotion will help cure dry skin on the lower legs, as symptoms will only get more severe, more visual, and more painful. While dry skin changes are the first warning sign of vein disease, other symptoms include: – Aching legs – Tiredness in the legs – Itchy, flaky, irritated dry skin 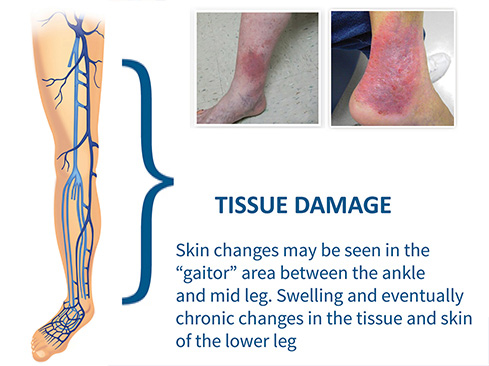 |
| Venous Ulcer | Leg ulcers can be a complication of venous disease. They are caused by long-standing venous insufficiency. Venous leg ulcerations are shallow, irritating, painful and typically found on the sides of the lower leg and around the ankle bone. We see them generally below the calf at the ankle or foot. What Are the Signs of Leg Ulcers? The first signs of leg ulcers may be dark, reddish-brown or purple skin discoloration with dry, firm skin in the lower leg. Chronic swelling in the ankle area may also be visible. When these signs and symptoms of pressure or aching go untreated, an ulcer can occur. Leg ulcers rarely occur quickly unless there is trauma, like dropping something on or hitting the skin. That’s good news because once you recognize the impending signs of ulcers, you should have adequate time to get the proper treatment before they form and become a chronic sore with pain which oozes fluid. If you see the warning signs of ulcers, reach out to a vein care specialist today to discuss the best treatment before they become a bigger problem. |
||
| CHRONIC VENOUS INSUFFICIENCY(ALSO CALLED Phlebitis, Post-Thrombotic Syndrome, Venous Insufficiency, Venous Leg Ulcer) | |
| BY DR. PETER K. HENKE
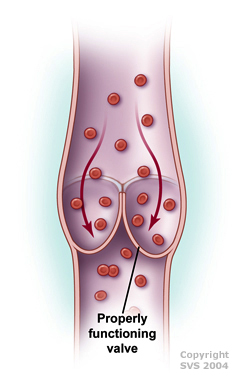
If you have CVI, valves in your veins (usually in the leg or sometimes the arms) don’t work, causing blood to pool in your legs and putting increased pressure on the walls of the veins. May be due to valve dysfunction (usually hereditary) or due to valve destruction after a deep vein thrombosis (DVT) or blood clot. |
 |
| DEEP VEIN THROMBOSIS | |
| BY DR. DEEPAK G. NAIR
Occurs when your blood thickens in a clump that becomes solid, forming a clot. Nearly 300,000 first-time cases of DVT occur in the U.S. every year, usually in the leg. REQUIRES PROMPT ATTENTION |
 |
| PERIPHERAL ARTERIAL DISEASE | |
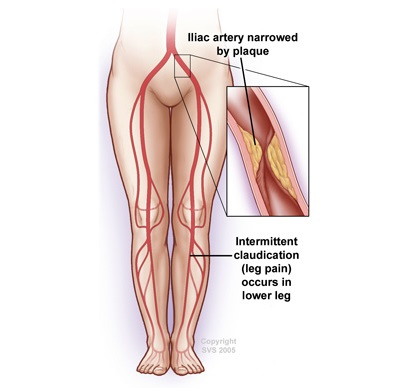
| ALSO CALLED PAD, peripheral vascular occlusive disease (PVOD), peripheral arterial occlusive disease (PAOD), “hardening” of the arteries, peripheral atherosclerosis
Edited by DR. KELLIE R. BROWN PAD is a chronic disease in which plaque builds up in the arteries to the legs. This buildup typically occurs gradually. If allowed to progress, blood flow in that artery can become limited or blocked all together. |
|
| AORTOILIAC OCCLUSIVE DISEASE | |
| BY DR. RAGHUVEER VALLABHANENI
Aortoiliac occlusive disease is the blockage of the aorta, the main blood vessel in your body, or the iliac arteries. The iliac arteries are the branches that your aorta divides into around the level of the belly button to provide blood to your legs and the organs in your pelvis. This blockage is typically caused by a buildup of plaque within the walls of your blood vessels. |
|
| LYMPHEDEMA | |
| BY DR. MANJU KALRA
Lymphedema is an accumulation of lymph fluid in the soft tissues, most frequently in the arms or legs. Lymph fluid, rich in protein, is normally filtered by the lymph nodes and is then released into the bloodstream. When the nodes are obstructed, their filtering capacity is overwhelmed and lymph fluid collects and causes swelling. |
|